LAPIP™ case study: Treatment of site #4 with peri-implantitis
Robert A. Levine, DDS, FCPP, FISPPS
Patient history
A 63-year-old male patient was referred in January 2015 after a routine cleaning at his restorative dentist’s office where the hygienist recorded pocketing and heavy bleeding upon probing around an implant in site #4. (figs 1-2) The Straumann RN TE implant was placed in 5/12/2003 under my care due to a previous root fracture of a root canal treated tooth that had been extracted by a local surgeon 6 months prior to presentation. The final crown was cemented with a polycarboxylate cement in 2003. The patient had been very compliant with regular every 6 months prophylaxis with his restorative dentist. The patient had a medical history of A-Fib and high cholesterol. Medications to control them included a statin, metoprolol, and warfarin. Parafunctional habits may have been contributory to the failed tooth. A nightguard appliance had not been recommended previously.
The patient was diagnosed with site-specific peri-implantitis around #4 and localized beginning-to-moderate periodontitis interproximal to #26-27 with probing depths of 5 to 7mm. Probing depths around #4 were buccally (distal to mesial) 7,7,9mm and lingually (mesial to distal) 9,7,7mm with heavy bleeding upon probing circumferentially with zero mm of visible facial recession recorded. The implant was not mobile, but there was bone loss on the mesial aspect to the third thread as noted on radiographic exam. (fig 1)
Treatment approach
After a presentation of treatment options, the patient accepted LAPIP treatment using the PerioLase® MVP-7™ Nd:YAG laser. The advantages of LAPIP treatment that factored into his decision were the ability to treat immediately in one surgical visit with minimal post-op discomfort along with the effectiveness of the Nd:YAG in reducing the subgingival bacterial load and thus controlling the localized infection, while minimizing post-operative recession (Richman et al 2020).
As the cement was not radiographically detected and the circumferential nature of the pocketing around the implant, the discussion with the patient was to reevaluate in 6 months for soft and hard tissue healing and if there would be a need to re-enter the area surgically for a GBR procedure.
LAPIP procedure was performed for #4 and LAR (laser assisted regeneration) completed for #2,3,5 (total of 542 joules used in the upper right sextant) and LAR #26,27 (total of 604 joules used) in February 2015 (fig 3). The patient experienced zero out of ten on a discomfort scale (1 to 10 in degree of discomfort) at his followup visit in 2 weeks immediately post-surgery.
Our LANAP/LAPIP office protocol is the following: visits every 2-3 weeks for a prophylaxis with a RDH with review of plaque control measures until 3 months post-procedure, followed by a 3-month periodontal maintenance protocol, eventually sharing responsibilities with the restorative dentist once the patient is periodontally stable. A maxillary nightguard appliance was recommended to control his parafunctional habits.
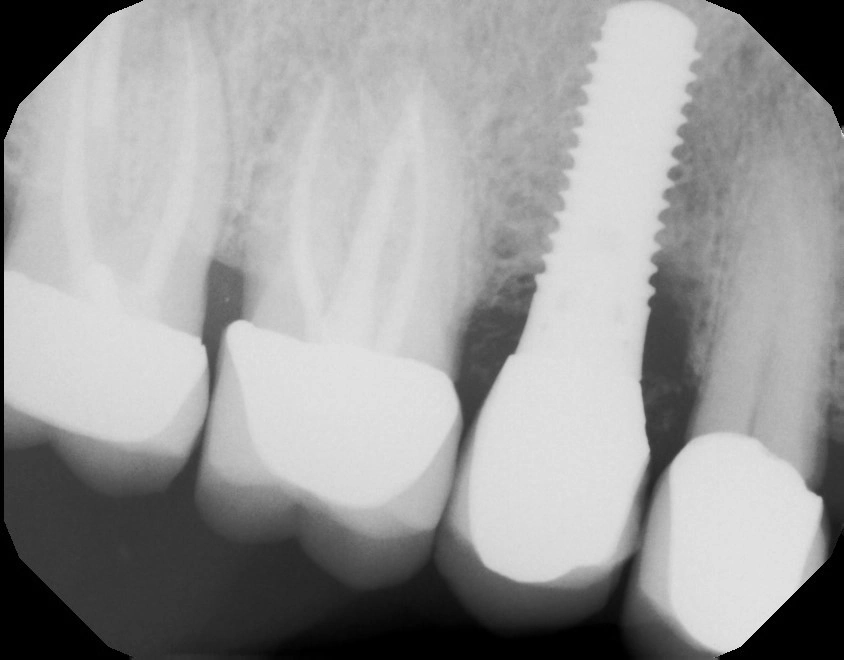
Fig. 1: Pre-op radiograph

Fig. 2: Pre-op clinical photo showing heavy BOP

Fig. 3: GE immediately post LAPIP treatment
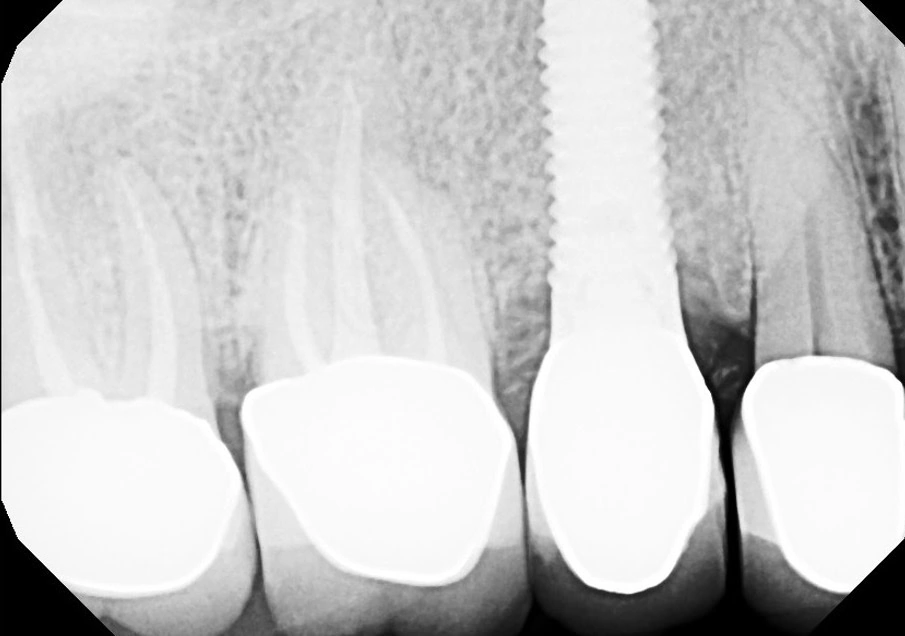
Fig. 4: 1 year post-op

Fig. 5: 7 year post-op
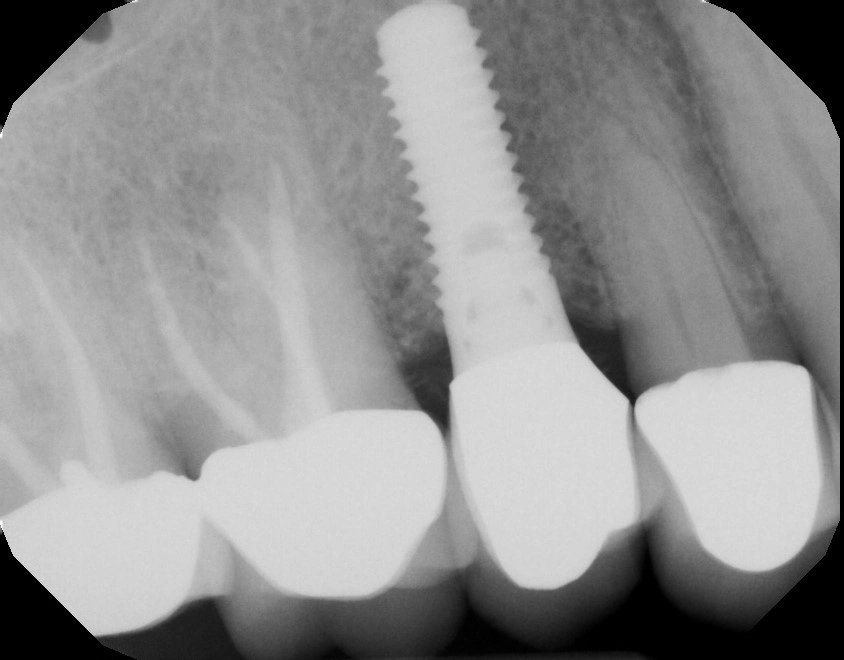
Fig. 6 7 year post-op
Results
One year post-op radiographs taken in July 2016 (fig 4) showed clear bone fill with decreased probing depths. No bleeding or suppuration were noted during post-op exams and the patient maintained good plaque control. The patient returned to the care with his restorative dentist for periodontal maintenance visits every 4-6 months.
The patient returned 6.5 years later for an extraction and dental implant for site #19 which was lost due to root fracture of a previously treated root canaled tooth.
A 7-year post-treatment exam (fig 5) and digital radiograph (fig 6) was completed in May 2022, indicating continued health of the implant and increased bone density and complete fill on the mesial and distal aspects. Probing depths were buccally: 4,2,4mm (distal to mesial) and 4,2,4 mm (mesially to distally) with light bleeding noted on the mesial aspect upon probing. No recession facially was noted associated with #4, however the natural tooth #5 recorded an additional 1 mm of buccal recession. The tissues appeared healthy for the upper right and lower anteriors at 7 years. He again expressed his pleasure and gratitude of our ability to treat and maintain his #4 implant non-surgically with the state-of-the-art advanced laser technology with the PerioLase® MVP-7™ Nd:YAG laser.

About the Author
Robert A. Levine, DDS
Dr. Robert A. Levine maintains a private practice in Philadelphia at the Pennsylvania Center for Dental Implants and Periodontics. He graduated from Temple University School of Dentistry, received his post-grad certificate in Periodontics from the University of Pennsylvania and is presently a Clinical Professor in Post-Graduate Periodontics and Dental Implantology at the Temple University Kornberg School of Dentistry, and has clinical appointments at the University of North Carolina School of Dentistry at Chapel Hill and the University of Illinois College of Dentistry at Chicago.
Dr. Levine is a Diplomate of the American Board of Periodontology, Fellow, and President of the International Society of Periodontal Plastic Surgeons (FISPPS), a Fellow, and Board of Directors of the Academy of Osseointegration (AO), and Fellow, and US Section Membership Coordinator for the International Team for Implantology (ITI). He has lectured extensively and presently serves on the Editorial Boards of numerous international scientific dental journals and has authored over 90 professional publications.
