LANAP® case study
Harinder Sandhu, DDS
Patient History
A 50-year-old Caucasian female was referred for treatment of severely advanced periodontitis, complaining about bleeding gums and splaying of maxillary anterior teeth. The patient’s health history was unremarkable other than that she is on anti-depressants. Intraoral examination showed highly inflamed gingival unit with periodontal abscess on #11(9), 26(14), and 42(26). Cross bite on #26(14) and extrusion of #11,12 from its socket (8,9) with a diastema of 4 mm between maxillary central incisors. Right maxillary central and lateral incisor had mobility of grade II; all maxillary molars had class II furcation invasion. She was devastated about the prospect of losing her maxillary anterior teeth. Radiographs showed advanced horizontal bone loss on maxillary anterior teeth and angular intraosseous defects on M #26(14) and M #35(20). Pocket depths ranged from 3-15 mm.

Treatment approach
The patient was diagnosed with generalized severely advanced chronic periodontitis (Stage III, Grade 2), with splaying of maxillary anterior teeth and cross bite on #26(14). She was sent for medical evaluation for type 2
diabetes, which was negative. Full-mouth LANAP® Protocol was started 15 June 2018. Full-mouth orthodontic rehabilitation was recommended, however, due to financial concerns she only opted for limited orthodontic treatment on maxillary teeth. Orthodontic treatment was initiated six months after LANAP® treatment and consisted of lateral movement of maxillary anterior teeth. The patient was followed up during her orthodontic treatment and occlusal adjustment was done at all maintenance visits, which were scheduled every three months.
Results
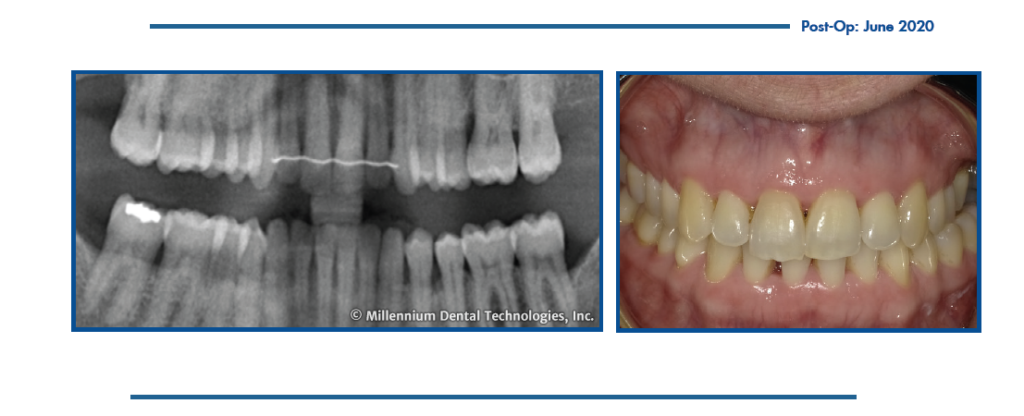
The patient was compliant and presented as per protocol at the 1, 3, 6 and 9-month visits. During those visits, we observed decreased gingival redness, absence of suppuration, decreased mobility and radiographic evidence of new bone.
At the 12-month visit, signs of inflammation were minimal, except for the posterior teeth that had been considered hopeless where bleeding on probing was still present. No mouth odor was present. Teeth #2, 3, 17, and 18 had class 1 mobility, and the remaining teeth showed no mobility and none of the teeth were depressible. At multiple sites, we observed horizontal bone growth radiographically.
Two years after the initiation of LANAP® Protocol, full-mouth probing showed pocket depths reduced to 2-3 mm. Significant bone level increase was noted visually in maxillary anterior area, on mesial of left maxillary first molar, on left mandibular second premolar, as well as in Q4. The patient remains stable on a three-month maintenance program.

About the Author
Harinder Sandhu, DDS, PhD
Dr. Sandhu received his initial dental training from Guru Nanak University in India, his Ph.D. in Anatomy in 1982 from the University of Ottawa, and a Certificate in Periodontics in 1985 from Loma Linda University. Dr. Sandhu started as a faculty member at Western University in 1985 and served as Director and Vice-Dean of Schulich Dentistry at Western University; Chair of the Periodontics Division; and the Chair of the Admissions Committee in Dentistry.
Dr. Sandhu has been a prolific researcher, especially in the area of periodontics, resulting in numerous academic awards and invitations to provide lectures on Periodontology worldwide. In Jan 2023, he became the Elected President of the Royal College of Dental Surgeons Ontario (RCDSO). He has been recognized as a Fellow by the American College of Dentists and the International College of Dentists, Pierre Fauchard Academy, and the International Academy of Dentistry. Dr. Sandhu is an impassioned proponent of accessibility of oral health care to under-serviced populations.
